Treatments
- Diseases
- AsthmaAsthma
- COPDCOPD
- Interstitial Lung DiseaseInterstitial Lung Disease
- PneumoniaPneumonia
- Sleep ApneaSleep Apnea
- Bronchitis & Chronic CoughBronchitis & Chronic Cough
- Pulmonary FibrosisPulmonary Fibrosis
- TuberculosisTuberculosis
- SarcoidosisSarcoidosis
- Lung Cancer EvaluationLung Cancer Evaluation
- Pleural EffusionPleural Effusion
- PneumothoraxPneumothorax
- Pulmonary EmbolismPulmonary Embolism
- ARDSARDS
- Allergic Lung DiseasesAllergic Lung Diseases
- Post-COVID Lung DiseasePost-COVID Lung Disease
- Occupational Lung DiseasesOccupational Lung Diseases
Allergic Lung Diseases
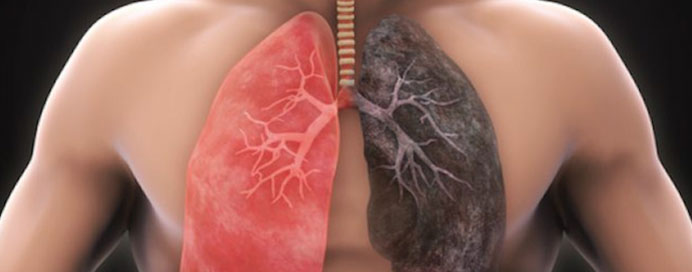
Allergic Lung Diseases are a group of respiratory conditions triggered by exposure to allergens such as dust mites, pollen, mold, animal dander, or certain occupational particles. These allergens cause the immune system to overreact, leading to airway inflammation, mucus buildup, coughing, wheezing, and breathlessness. Conditions like allergic asthma, hypersensitivity pneumonitis, and allergic bronchopulmonary aspergillosis (ABPA) fall under this category. Early diagnosis and avoidance of triggers are essential to prevent flare-ups and long-term lung damage.
Common Types of Allergic Lung Diseases
- Allergic asthma caused by environmental triggers like pollen, dust, and pollution.
- Hypersensitivity pneumonitis due to repeated exposure to organic particles (birds, mold).
- Allergic bronchopulmonary aspergillosis (ABPA) caused by fungal sensitization.
- Seasonal allergic rhinitis progressing to lower airway irritation.
- Occupational lung allergies triggered by chemicals, latex, or industrial dust.
Symptoms & Clinical Features
- Recurrent coughing, especially at night or early morning.
- Wheezing and whistling sounds while breathing.
- Shortness of breath, chest tightness, and reduced exercise tolerance.
- Persistent nasal congestion, sneezing, or itchy eyes associated with allergens.
- Episodes worsened by weather changes, dust exposure, pets, or workplace irritants.
Diagnosis & Management
- Allergy testing (skin prick tests or IgE levels) to identify specific triggers.
- Pulmonary function tests to assess airway obstruction or restriction.
- Medications like inhaled corticosteroids, antihistamines, and bronchodilators.
- Environmental control: air purifiers, dust protection, mold removal, and avoiding triggers.
- Advanced therapies like immunotherapy (allergy shots) for long-term tolerance building.